Modernizing Claims Administration: 50% Cost Reduction for a Leading Dental Insurer
Claims processing in dental insurance is often riddled with manual steps, fragmented systems & legacy tech that lead to delayed and inaccurate claim adjudication & payments. For one dental insurer, these inefficiencies not just in claims processing but also provider onboarding weren’t just painful—they were expensive.
That’s where LightSpun came in.
We deployed our end-to-end claims platform to transform their operations --> cutting administrative costs by 50% while improving accuracy, transparency, and speed across the board.
🔧 The Challenge
This insurer faced three core problems:
- Outdated Claims System: Multiple disconnected legacy systems made it difficult to accurately adjudicate claims and track claim status or identify delays.
- Paper Intake Bottlenecks: A significant percentage of claims were still received by mail, fax or email, requiring manual data entry.
- Credentialing Delays: Verifying provider eligibility often took months, holding up claims and payments.
🚀 The LightSpun Solution
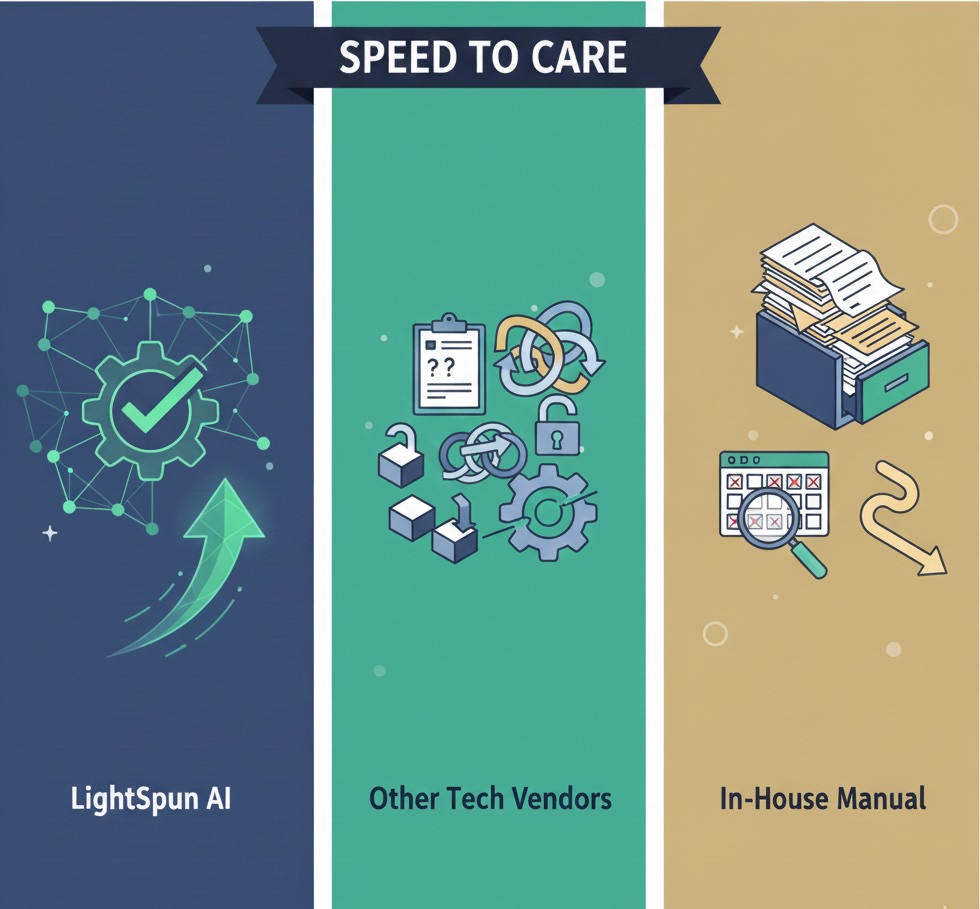
We replaced their multiple systems with a single, AI-powered platform that handles intake, adjudication, and payment—all in one workflow.
Here’s what we deployed:
✅ Claims System Modernization
Our digital claims engine replaced their patchwork of tools. It automatically adjudicates claims in real-time, flags inconsistencies, and integrates seamlessly with their provider data.
✅ Paper Intake Automation
We digitized the paper and fax intake process using LightSpun’s AI agents. What once took hours of manual processing now takes minutes—completely integrated into the digital workflow.
✅ Provider Credentialing
We implemented our AI-powered credentialing module to primary source verify license, sanctions, NPI, and more. This not only ensured accuracy but also reduced their provider onboarding time.
📊 The Results
- 50% reduction in overall claims administration costs
- Faster claim turnaround time (from weeks to days)
- 99% of paper claims electronically adjudicated
- 95% claim auto-adjudication rate
- Providers onboarded in days, not months
💡 Why It Matters
For payors, inefficiencies in claims and credentialing aren’t just operational headaches but they directly impact member experience, provider satisfaction, and bottom-line performance.
By consolidating claims administration & credentialing into one AI-driven system, LightSpun helped this insurer move from reactive to real-time.
Want to see how we can do the same for your organization? Schedule a demo
.jpg)