Claims Administration and Adjudication
Use configurable workflows to automate claims administration and adjudication workflows in your organization.
Automate Claims with Confidence
Streamline your entire claims lifecycle: from intake to payment with AI-powered automation. LightSpun ensures fast, accurate, and rules-driven adjudication, reducing costs and eliminating manual errors. Scale operations effortlessly while improving provider and member satisfaction.
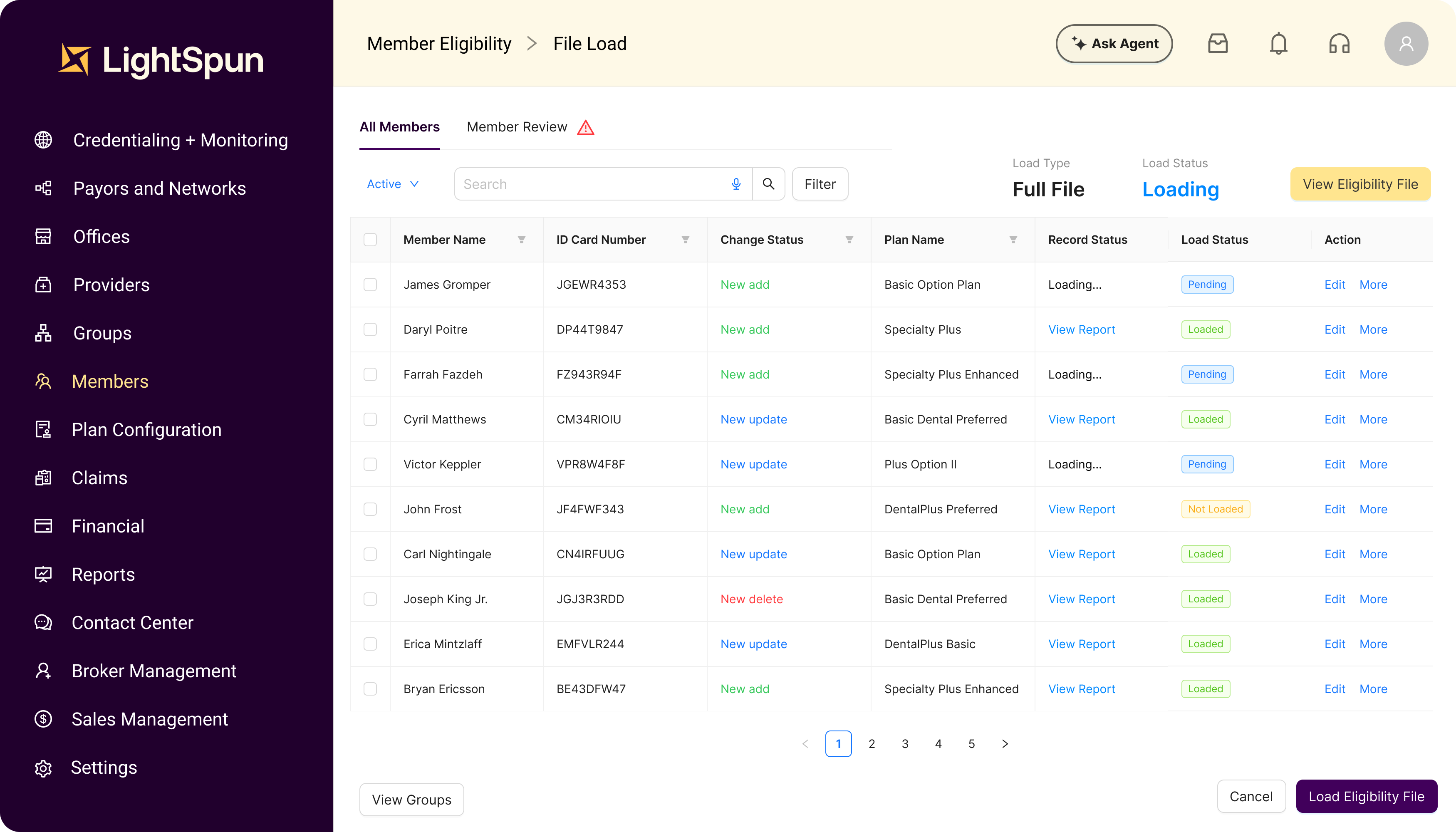
Flexible Eligibility Management
Intake, resolve and standardize member eligibility files from multiple data sources (EDI 834, CSVs etc).
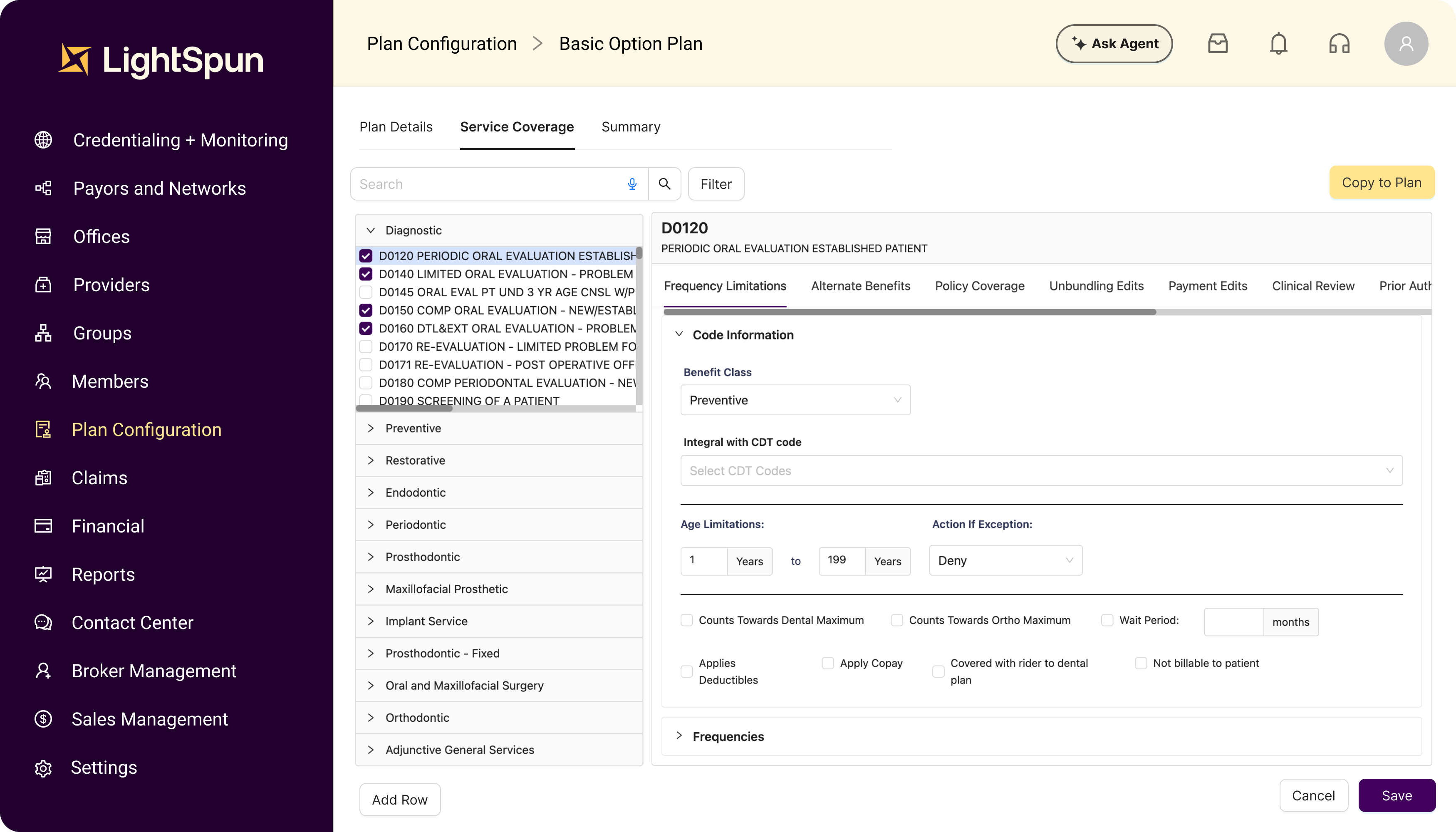
Plan
Configuration
Reduce the complexity of configuring, loading and managing bundled plans for commercial, individual and government plans.
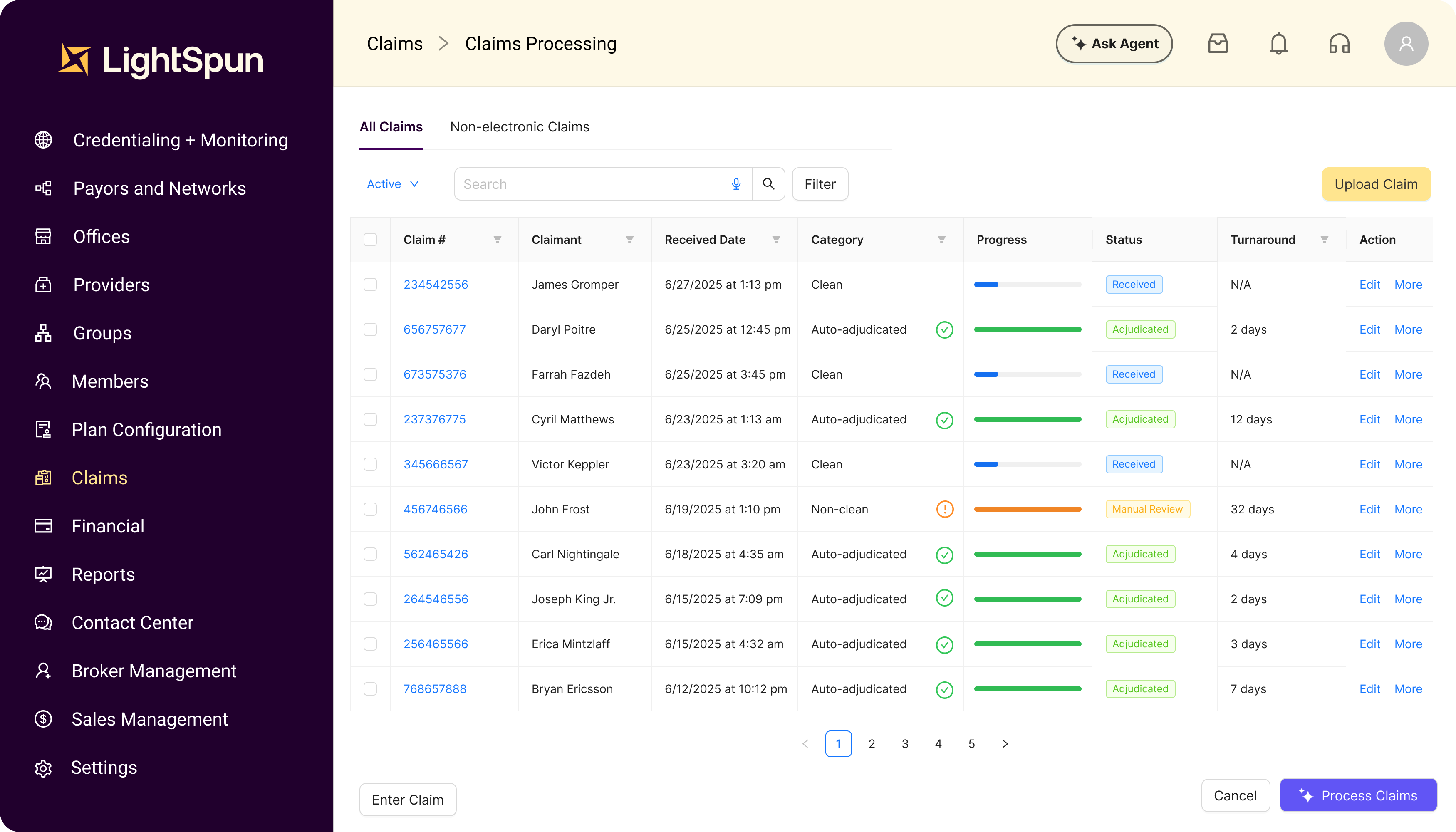
Automate Claims with EDI Standards
Integrate with clearinghouses using EDI standards (e.g. 837, 834, 270/271, 276/277) and automate mail rooms/fax/email claims using AI to auto adjudicate claims

Reporting
& Insights
Real-time insights that go beyond predictive to prescriptive for operating and financial metrics such as claims payout, loss ratios, utilization reviews, provider metrics and membership trends.
Get claims processed faster — with AI doing the heavy lifting
Intake and manage provider directory, multiple networks and fees for claim adjudication
Create, configure and administer payment, billing, premiums, receivables and payables for all groups and plans
Manage and monitor state and federal compliance regulations with a SOC-2 Type II certified platform
Trusted by clients
Unlock your organization's full potential
Partner with Lightspun to make transformational changes to your organization. Our unified platform helps our customers achieve lasting results through intelligent automation, reduced processing time, and enhanced provider network management.