Provider Network Management
Optimize end-to-end provider network management for Payors from recruiting and contracting to credentialing, recredentialing, and compliance with NCQA standards
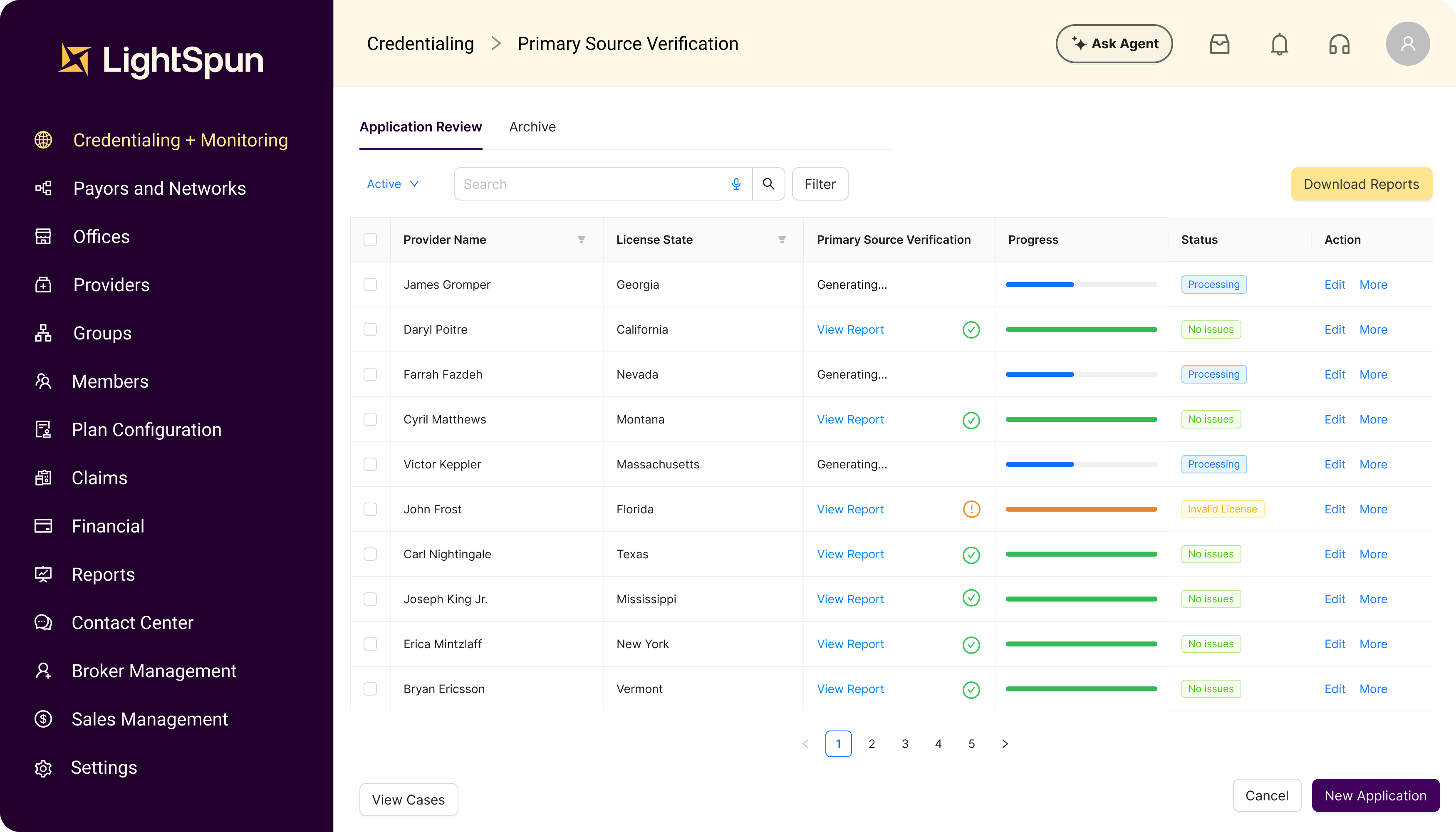
Reduce administrative costs associated with managing and credentialing your provider network
Enable provider self-service through a modern portal that accelerates data intake and reduces administrative workload
API
Ingest data via our CAQH API to improve timeliness and completeness of provider profiles
Automate workflows and routing with configurable queues, templated documents, and centralized case tracking
Ensure compliance with real-time reporting for directory verification, roster management, and credentialing status
Trusted by clients
Unlock your organization's full potential
Partner with Lightspun to make transformational changes to your organization. Our unified platform helps our customers achieve lasting results through intelligent automation, reduced processing time, and enhanced provider network management.