Dental insurers in Connecticut are facing a new mandate: prove that at least
83% of every premium dollar goes toward actual patient care—or pay rebates to policyholders. And it’s not just Connecticut. A dozen-plus states are moving forward with similar laws or reporting requirements, from Massachusetts (whose 83% DLR law
transformed its market) to Alabama, Kansas, New York, and West Virginia.
Why It Matters
These regulations, known as dental loss ratio (DLR) laws, are designed to ensure premiums actually fund patient care, not administrative overhead. That’s a major pressure point for an industry still spending nearly 18% of every dollar on faxes, paper claims, and legacy admin processes.
For insurers, failure to modernize isn’t just inefficient—it’s risky. Falling short of DLR targets can trigger compliance penalties, drive up premiums, and erode trust among members and providers.
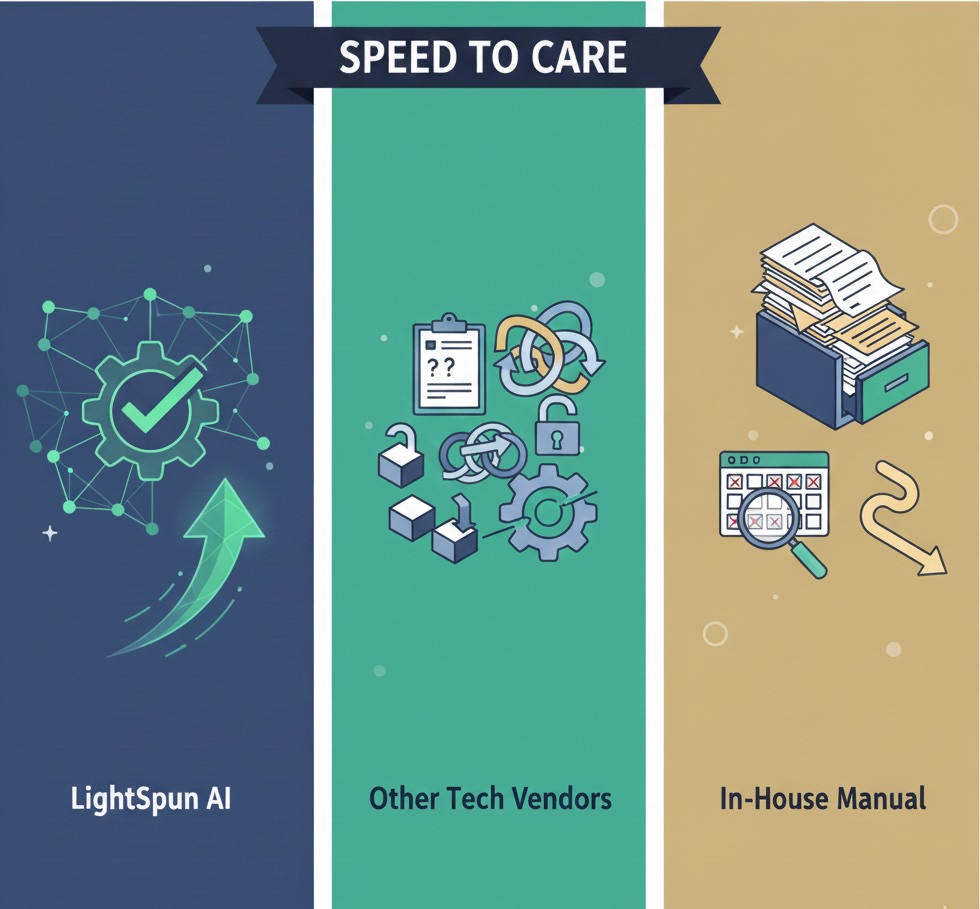
How Lightspun Helps
Lightspun was built for this moment. Our AI-native claims platform automates adjudication and drastically cuts administrative waste:
- 90%+ of claims auto-adjudicated, reducing manual review
- Administrative costs cut in half, thanks to fully digital workflows
- Paper claims nearly eliminated, improving speed and accuracy
With Lightspun, insurers can align with state DLR requirements, reduce operating costs, and redirect more premium dollars toward patient care—exactly what regulators and members want.
The Future Is Already Here
In Massachusetts, DLR laws are no longer hypothetical—they’ve redefined the market. More states are right behind. Lightspun equips insurers and providers with automation powerful enough to stay compliant, stay competitive, and put care—not paperwork—first.
Read more about the DLR movement here.

.jpg)