Provider Data Management
Streamline provider data and credentialing operations - including filling insurance applications - for DSOs and Group Practices, with full compliance to NCQA and payor requirements
Centralized Provider & Office Data Management
Centralize provider and office data with tools to manage complex location, network, and association relationships
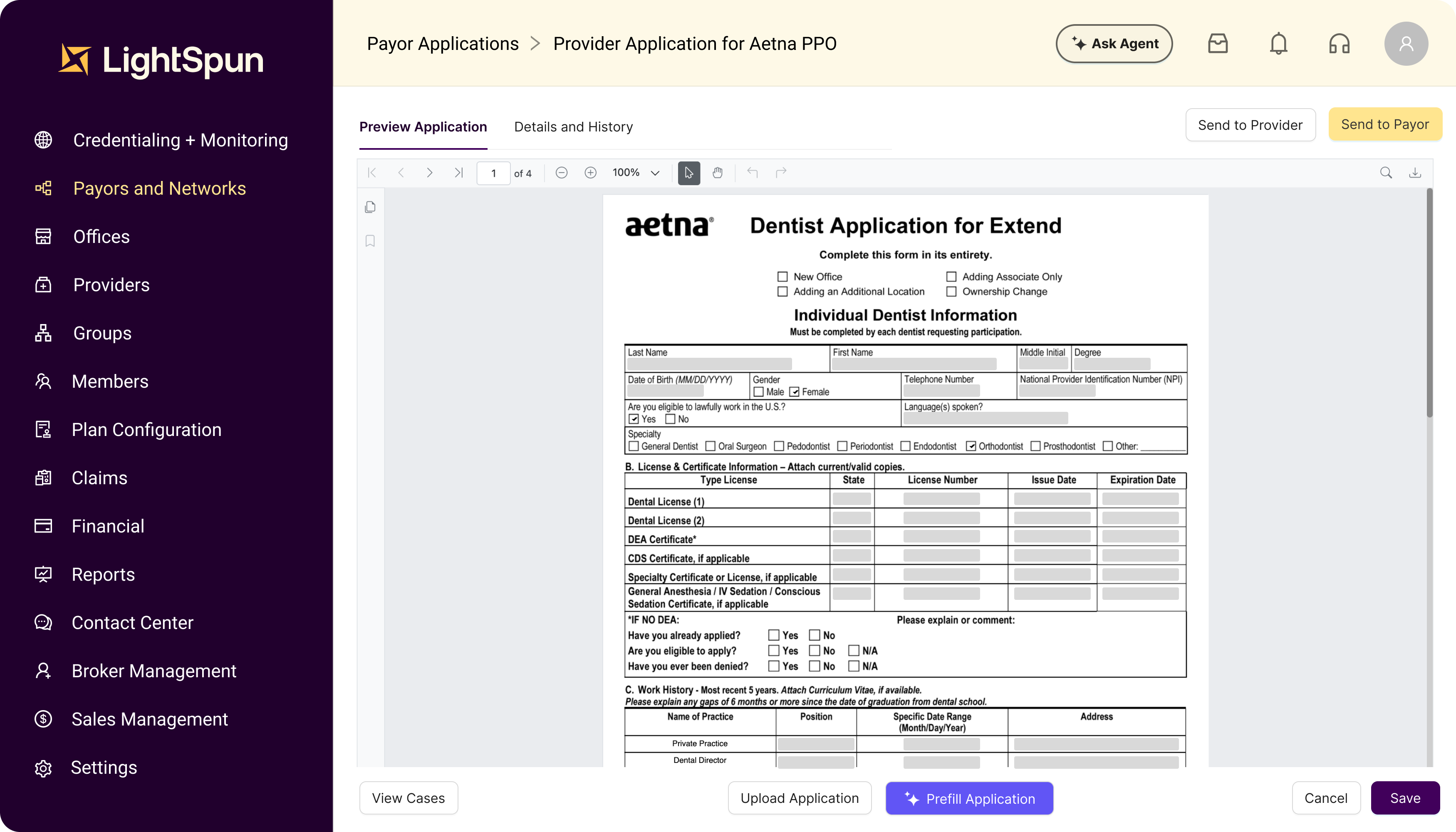
Automated Insurance Applications
Auto-fill payor applications using AI to complete and submit forms with the correct supporting documents
AI Powered Credentialing & Recredentialing
Streamline credentialing and recredentialing with automated primary source verification, sanctions monitoring, and license validation
Onboard your providers on the payor network in days instead of months
$50K - $100K
Incremental revenue per provider
80%
Reduction in credentialing time
50%
Reduction in manual error
Self-Service
Provider Portal
Provider Portal
Enable provider self-service with a portal that enables data and document collection while reducing staff burden
CAQH
API
API
Retrieve data from CAQH via real-time API integration to accelerate onboarding
Workflow Automation & Configurable Queues
Automate workflows and queueing using centralized tools for communications, documents, and case handling
Reporting & Compliance
Stay audit-ready with real-time access to compliance reporting across credentialing, rosters, and directories